
Throughout history, infectious disease and worst pandemics in the history has killed more human beings than any other cause. In recent times The World Health Organization has declared COVID-19 a pandemic. This is a breakthrough event. As human civilizations bloomed, so did infectious disease. Civilizations demand proximity to large numbers of people living with each other and domestic animals. This provided the fertile breeding grounds for the disease, often with poor sanitation and nutrition. And new overseas trading routes spread the new infections far and wide, creating the first global pandemics.
Let’s go deeper into the field of world’s breakthrough event – and take time to read through about Outbreak, Epidemics, and Pandemic.
A Glimpse Of Idea On The Outbreak, Epidemics, And Pandemics:
As human civilizations bloomed, so did infectious disease. Civilizations demand proximity to large numbers of people living with each other and domestic animals. This provided the fertile breeding grounds for the disease, often with poor sanitation and nutrition. And the new overseas exchange routes spread the novel infections far and wide, which create the first global pandemics.
In recent times The World Health Organization has declared COVID-19 a pandemic. This is a breakthrough event.
We have used this word pandemic around the world, but you might notice that some of us mixing up three important words & those are: Outbreak, Epidemic, and Pandemic.
Simply put, the difference between these three expansions of disease spread is a matter of scale.
Outbreak- It’s small but unusual.
By following diseases over time and geography, epidemiologists learn to estimate how many cases of illness should generally happen within a defined period, place, and population. An outbreak is a visible, often small, increase over the estimated number of cases.
An outbreak occurs with a sudden rise in the number of cases of a disease. An outbreak may happen in a community or geographical area or may affect numerous countries. It may generally last for a few days or maybe a week, or even for some years.
Some of the outbreaks are expected to occur each year, such as influenza. Sometimes a particular case of an infectious disease may be measured as an outbreak. This may be accurate if the disease is rare (e.g., foodborne botulism) or has severe public health implications (e.g., bioterrorism agents such as anthrax).
Take an example of an unusual spike in the number of children with diarrhea of a daycare. In this case, one or two sick kids might be usual in a typical week, but if 15 children in daycare got to catch with diarrhea all at a time, that is an outbreak.
When a new disease appears, outbreaks are more noticeable since the estimated number of illnesses caused by that disease was zero. Take the example of the cluster of pneumonia cases that sprung up unpredictably among market-goers in Wuhan, China. The Public health officials know the spike in pneumonia cases there established an outbreak of a new type of coronavirus, then named as SARS-CoV-2.
Epidemic- It’s greater and spreading.
An epidemic is an outbreak that spread over a larger geographic area, and an epidemic happens when an infectious disease spreads quickly to many people. When people in places outside of Wuhan started testing positive for infection with SARS-CoV-2 (which causes the disease known as COVID-19), epidemiologists recognized that the outbreak was spreading, a possible indication that containment efforts came too late or insufficient. This was not unpredicted, given that no treatment or vaccine is available yet. But widespread cases of COVID-19 across China recognized that the Wuhan outbreak had grown to an epidemic.
Pandemic-It’s International and without any control.
In the most standard logic, once an epidemic spreads to multiple countries or regions of the world, it is measured as a pandemic. Some epidemiologists classify a condition that a pandemic only once the disease is constant in some of the newly affected regions via local transmission.
To illustrate, a sick traveler with COVID-19 who returns to the U.S. from China doesn’t make a pandemic, but once they infect a few family members or friends, there’s some debate. If new local outbreaks ensue, epidemiologists will agree that efforts to control global spread have failed and refer to the emerging situation as a pandemic.
History of Pandemics
As humans have extended across the world, this supports to spread of infectious diseases. Even outbreaks are nearly frequent in this modern era, though every outbreak does not reach the pandemic level as the Novel Coronavirus (COVID-19) has.
This table shows history’s most deadly pandemics, from the Antonine Plague to the current COVID-19 event.
Timeline of worst pandemics in history:
| Pandemic Name | Time period | Approximately Death Toll |
| Antonine Plague | 165-180 | 5M |
| Japanese smallpox epidemic | 735-737 | 1M |
| Plague of Justinian | 541-542 | 30-50M |
| Black Death | 1347-1351 | 200M |
| New World Smallpox Outbreak | 1520 – onwards | 56M |
| Great Plague of London | 1665 | 100,000 |
| Italian plague | 1629-1631 | 1M |
| Cholera Pandemics 1-6 | 1817-1923 | 1M+ |
| Third Plague | 1885 | 12M (China and India) |
| Yellow Fever | Late 1800s | 100,000-150,000 (U.S.) |
| Russian Flu | 1889-1890 | 1M |
| Spanish Flu | 1918-1919 | 40-50M |
| Asian Flu | 1957-1958 | 1.1M |
| Hong Kong Flu | 1968-1970 | 1M |
| HIV/AIDS | 1981-present | 25-35M |
| Swine Flu | 2009-2010 | 200,000 |
| SARS | 2002-2003 | 770 |
| Ebola | 2014-2016 | 11,000 |
| MERS | 2015-Present | 850 |
| COVID-19 | 2019-Present | 1.7M Dec12,2020 (still tolling) |
7 of the worst pandemics in history & the end story
For many years scientists and medical researchers have differed over the exact definition of a pandemic; the confusion was whether it was a pandemic or an epidemic. Still, everyone agrees one thing, and that is, the word describes the widespread occurrence of disease over what might generally be expected in a different geographical area.
Plague, cholera, smallpox, and influenza are some of the most ruthless killers in human history. Besides, these diseases’ outbreaks across international borders are accurately defined as Pandemic, mostly smallpox, which has taken away between 300-500 million people in its 12,000-year survival throughout history.
Here’s how 7 of the world’s worst pandemics finally ended.
List of & worst pandemics in History:
- ANTONINE PLAGUE (165-180 AD).
- BLACK DEATH (1347-1351).
- SMALLPOX (1520- continue).
- CHOLERA (1817-1923).
- Spanish Flu (1918-1920).
- AIDS (1981-present day).
- H1N1 Swine Flu (2009-2010).
1. ANTONINE PLAGUE (165-180 AD) — Loss of Life was Incredible

Antonine Plague is also known as the Plague of Galen. This ancient pandemic affected mainly Asia Minor, Egypt, Greece, and Italy and has been either Smallpox or Measles. However, the actual cause is still unidentified. This mysterious disease was carried to Rome by soldiers returning from Mesopotamia around 165AD; unintentionally, they helped spread a disease that would kill over 5 million people and destroy the Roman army.
With the death of Marcus Aurelius, the Antonine plague also died down. Upon its wake, 10% of Rome’s population perished. But it did not end all in 180. Just nine years after it died down, it suddenly reappeared and continued to collect lives up until 270.
2 BLACK DEATH (1347-1351) — The Discovery of Quarantine

The plague never went away, and when it repeated 800 years later, it was killed with reckless abandon. The Black Death, which occurred in Europe in 1347, took an astonishing 200 million lives in just four years.
To find the way of stopping the disease, people still had no scientific understanding of contagion, says Mockaitis, but they identified that it had something related to proximity. That’s why intelligent thinker officials in the Venetian-controlled port city of Ragusa declared newly arrived sailors in isolation until they prove them fit & fine to back inland.
First of all, sailors had to stay on their ships for 30 days, which became known in Venetian law as a Trentino. As time passed, the Venetians prolonged the forced isolation to 40 days or quarantine, the word quarantine’s origin, and the beginning of its practice in the Western world.
“That affected,” says Mockaitis.
3 SMALLPOX (1520- continue) —A European Disease Results the New World

Smallpox was occurred as endemic to Europe, Arabia, and Asia for centuries. This persistent menace killed three out of ten people it infected and left the rest with pockmarked scars. Nevertheless, the death rate in the Old World paled in comparison to the destruction wrought on inherent people in the New World when the smallpox virus arrived in the 15th century with the first European travelers.
This virus cut them down by the tens of millions, as the indigenous peoples of our modern-day, the United States, and Mexico had zero natural immunity to smallpox.
Mockaitis says, “There hasn’t been a kill off in human history to match what happened in the American 90 to 95 percent of the indigenous population extinct over a century.” and “Mexico goes from eleven million people pre-conquest to one million.”
Then Centuries later, the virus of smallpox turned the first epidemic to be ended by a vaccine. In the later part of the 18th-century, Dr. Edward Jenner, a British doctor, revealed that milkmaids infected with a milder virus called cowpox seemed immune to smallpox. He legendarily inoculated his gardener’s 9-year-old son with cowpox and then exposed him to the smallpox virus with no ill effect.
Dr. Edward Jenner wrote in 1801, “The annihilation of smallpox is the most terrible scourge of the human species, must be the result of this practice.”
He was finally right. It took almost two more centuries, but in 1980 the World Health Organization (WHO) declared that smallpox had been entirely eradicated from the face of the Earth.
4 CHOLERA (1817-1923)—The Success Story of Public Health Research
Cholera devastated England, killing tens of thousands in the early- to the mid-19th century. The day’s prevailing scientific theory believed that the disease was spread by foul air, which was known as a “miasma.” However, a British doctor named John Snow assumed that the mysterious illness, which killed its victims within days of the first symptoms, lurked in London’s drinking water.
Snow acted like a scientific Sherlock Holmes, observed hospital records and morgue reports to track devastating outbreaks’ exact locations. He generated a geographic chart of cholera deaths over ten days. He initiated a cluster of 500 fatal infections adjacent to the Broad Street pump, a renowned city well for it’s drinking water.
Snow wrote, “As soon as I became familiar with the situation and range of this irruption (sic) of cholera, I assumed some contamination of the water of the much-frequented street-pump in Broad Street.”
With diligent effort, Snow succeeded to convince local officials to take away the pump handle on the Broad Street drinking well, rendering it unusable the infections dried up, it’s work magically. Snow’s work didn’t cure cholera overnight; then again, it eventually led to a global effort to develop urban sanitation and protect drinking water from contamination.
While cholera has mostly been eliminated in developed countries, it’s still a persistent killer in third-world countries where they lack adequate sewage treatment and access to clean drinking water.
5 Spanish Flu (1918-1920) — Actually, it did not originate in Spain
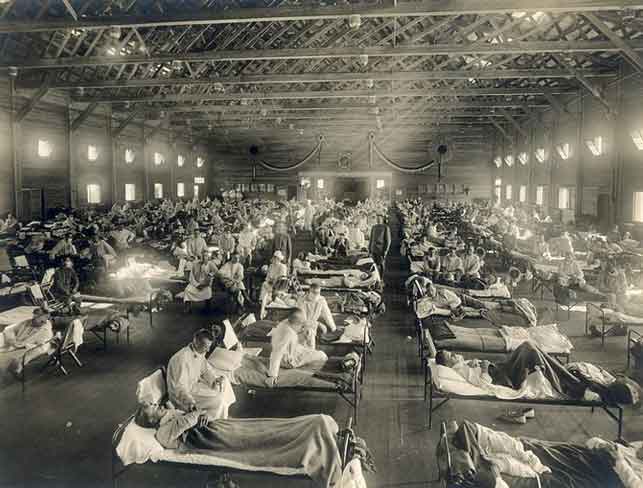
Spanish Flu victimized an estimated 500 million people from the South Seas to the North Pole. One-fifth of those died, with some native communities pushed to the brink of extinction. The Flu’s spread and lethality were boosted by soldiers’ cramped conditions and poor wartime nutrition that many people were suffering during World War I.
Though the name Spanish Flu, the disease probably did not begin in Spain. Instead, Spain was a neutral nation during the war and did not impose severe censorship of its press, freely publishing early counts of the illness. That is why; people misleadingly believed the sickness was specific to Spain, and the name Spanish Flu stuck.
In 1919, the flu pandemic was ended, as those infected either died or developed their strong immunity. And almost 90 years later, in 2008, researchers declared they’d discovered what made the 1918 flu so lethal: A cluster of three genes enabled the virus to deteriorate a victim’s bronchial tubes & lungs and then clear the way for bacterial pneumonia.
6 AIDS (1981-present day) — It’s both Pandemic and epidemic

We’re still battling with The HIV/AIDS pandemic, while medicine has made great strides, making HIV in many ways a chronic form that can manage in many countries, the end of the Pandemic quite a long way to go. In 1981 HIV/AIDS originated in Cameroon and was first recognized as a disease, while the earliest known case is believed to be in the Congo in 1959. AIDS had caught at least 60 million people, and 25 million had died in 2011.
Today its effect varies widely across the world—while in 2008, an estimated 1.2 million Americans had HIV, Sub-Saharan Africa alone was home to 22.9 million cases, with one in five adults are infected. About 38 million people were supposed to have HIV in 2018.
Estimation stated that AIDS had taken 35 million lives since it was first identified. The virus HIV causes AIDS, likely developed from a chimpanzee virus, then transferred to humans in West Africa in the 1920s. The virus, through its way around the globe and AIDS, was Pandemic by the late 20th century. About 64% of the projected 40 million living with human immunodeficiency virus (HIV) live in sub-Saharan Africa.
For decades, the disease had no recognized cure, but medication advanced in the 1990s allows people with the disease to experience an average life span with consistent treatment. Even more boosting, two people have been cured of HIV in early 2020.
7 H1N1 Swine Flu (2009-2010) — Key symptoms of swine flu in swine
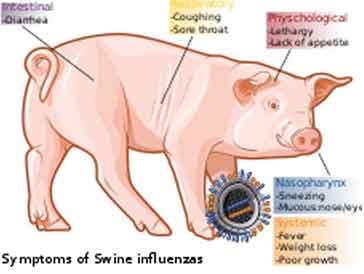
In 2009 swine flu pandemic was caused by a new strain of H1N1 that originated in Mexico before spread out to the rest of the world. According to the
Centers for Disease Control and Prevention (CDC), within one year, the virus-infected as many as 1.4 billion people worldwide and killed between 151,700 and 575,400 people.
The CDC reported that the 2009 flu pandemic mainly affected children and young adults, and 80% of the deaths were in people younger than 65. That was strange, considering that most flu viruses, including those that cause seasonal Flu, cause the maximum percentage of deaths in people ages 65 and older. However, in the swine flu, older people appeared to have already built up sufficient immunity to the group of viruses that H1N1 belongs to, so weren’t affected as much. A vaccine for the H1N1 virus that caused the swine flu is now being included in the annual flu vaccine.
Covid-19 shows how vulnerable we are
The world was introduced to a novel coronavirus—SARS-CoV-2—a pathogen that causes COVID-19 in late December 2019. Just two months later, the World Health Organization (WHO) declared the coronavirus outbreak to a pandemic, meaning the virus had spread across numerous countries and infected many people.
The COVID-19 pandemic is in its primary stages, and it is impossible to predict its future impact. This post and infographic are meant to provide historical context, and Covid-19 shows us how vulnerable we are – and how we can escape similar pandemics in the future.
People worldwide have become more aware of the best practices during this coronavirus pandemic, staring from careful hand-washing to social distancing. Countries across the globe accounted for mandatory stay-at-home measures, closing all offices, schools, businesses, and public places. Dozens of companies and many more independent researchers began working on tests, finding treatments, and vaccines. The eagerness for the human race to survive the pandemic became the primary concern in the world.
The consequence of the Covid-19 pandemic is unpredictable at the time of this writing. But we can learn from pandemics in history to define our best courses. These are our teachers – the Spanish flu, the AIDS pandemic, and more.
Flourished human civilizations & disease spreading
We arrived at where we began, increasing global connections and exchanges as a driving force behind all the pandemics. From the small hunting culture and gathering tribes to the metropolis, humanity’s dependence on one another has also generated disease opportunities to spread widely.
The blooming of urbanization in the developing world brings more and more rural residents into denser neighborhoods. At the same time, population growth puts enormous pressure on the earth’s resources. At the same time, the air movement of human passengers nearly doubled in the past decade. These functional trends are having an intense impact on the spread of infectious diseases.
The leading organizations and governments worldwide are asked to exercise social distancing to help ease the rate of infection, and the digital world is becoming a blessing for people to continue the connections and commerce like never before.
Common FAQs and facts about coronavirus (covid 19) Pandemic:

01 Is the coronavirus disease a pandemic?
COVID-19 can be considered as a pandemic. The reason is the rapid increase in the number of cases outside China over the past 2 weeks that has affected an increasing number of countries.
02 What is the difference between the coronavirus and the influenza virus?
The speed of transmission is an essential point of difference between the two viruses. Influenza has a shorter median incubation period- the time from infection to appearance of symptoms and a shorter serial interval- the time between successive cases than the COVID-19 virus. The serial range for the COVID-19 virus is projected to be 5-6 days. In contrast, in the influenza virus, the serial interval is three days. Then we can say that influenza can spread faster than COVID-19.
Additionally, transmission in the first 3-5 days of illness, or potentially pre-symptomatic transmission –transmission of the virus before the appearance of symptoms is a significant driver of influenza transmission. In other cases, while we are informing that several people can shed COVID-19 virus 24-48 hours earlier to symptom onset, currently, this does not appear to be a significant driver of transmission.
03 How do viruses get their name?
Based on their genetic structure, viruses are named to facilitate the development of diagnostic tests, vaccines, and medicines. Virologists and the wider scientific forum initiate this, so basically, viruses are named by the International Committee on Taxonomy of Viruses (ICTV).
04 The pandemic originated in Spain
No one believes the so-called “Spanish flu” originated in Spain.
The Pandemic likely entitled this nickname because of World War I, which was in full swing at this period. The powerful controlling countries involved in the war were keen to avoid exposing against their enemies, so reports of the Flu’s extent were repressed in Germany, France, Austria, the United Kingdom, and the U.S. By contrast. Neutral Spain had no interest in keeping the Flu under wraps. That created the wrong impression that Spain was bearing the brunt of the disease.
Though hypotheses have suggested, East Asia, Europe, and even Kansas, the Flu’s geographic origin is questioned.
05 The first wave of the pandemic was most lethal
The initial wave of deaths from the Pandemic in the first half of 1918 was comparatively low.
It was in the second wave; from October through December of that year recorded the highest death rates. And the third wave in the spring of 1919 was more lethal than the first but less so than the second.
Scientists now consider that the marked increase in deaths in the second wave was caused by conditions that favored the spread of a deadlier strain. People with mild cases stayed home, but those with severe cases were often crowded together in hospitals and camps, increasing the transmission of a more lethal form of the virus.
06 How long will the coronavirus pandemic last?
A pandemic defiantly will not be a short, sharp event. Actually, a pandemic may come in several waves over 12 months or more—this is typical of influenza pandemics. Yet we don’t know how long the COVID-19 pandemic will last, but we should be ready to have the coronavirus in some way in our lives for the next 9 to 12 months. It might be less, or it might be longer.
07 How can countries respond to a pandemic?
When an outbreak of disease reaches to pandemic levels, as COVID-19- there is typically a move away from outbreak containment, which centers on preventing transmission, to outbreak mitigation, which focuses on slowing and reducing the adverse effects of transfer. We should expect to face a mixture of containment and mitigation measures used by different countries around the world at a different time.
08 What causes a pandemic?
Several factors can cause pandemics. For example, in some cases, a new strain or subtype of virus that first emerged in animal’s catches humans and then becomes readily transmissible between humans. In other instances, an existing disease-causing agent mutates, increasing its infectiousness.
09 How do pandemics end?
Pandemics usually slow and come to an end on their own. However, the process may be speeded up through effective preventive strategies, such as improved personal hygiene or a vaccine’s progress. Some pandemics, though, occur in waves, such that decreased disease activity may be followed by another period of high disease prevalence, thus prolonging the outbreak.
Reference: